Nature Genetics, Aug 2022
A Rouf Banday # , Megan L Stanifer # , Oscar Florez-Vargas # , Olusegun O Onabajo , Brenen W Papenberg , Muhammad A Zahoor , Lisa Mirabello , Timothy J Ring , Chia-Han Lee , Paul S Albert , Evangelos Andreakos , Evgeny Arons, Greg Barsh , Leslie G Biesecker , David L Boyle , Mark S Brahier, Andrea Burnett-Hartman, Mary Carrington, Euijin Chang, Pyoeng Gyun Choe, Rex L Chisholm, Leandro M Colli, Clifton L Dalgard, Carolynn M Dude, Jeff Edberg, Nathan Erdmann, Heather S Feigelson, Benedito A Fonseca, Gary S Firestein, Adam J Gehring, Cuncai Guo, Michelle Ho , Steven Holland , Amy A Hutchinson, Hogune Im, Les'Shon Irby, Michael G Ison, Naima T Joseph, Hong Bin Kim, Robert J Kreitman, Bruce R Korf, Steven M Lipkin, Siham M Mahgoub, Iman Mohammed, Guilherme L Paschoalini, Jennifer A Pacheco, Michael J Peluso, Daniel J Rader , David T Redden , Marylyn D Ritchie, Brooke Rosenblum, M Elizabeth Ross, Hanaisa P Sant Anna, Sharon A Savage, Sudha Sharma, Eleni Siouti, Alicia K Smith, Vasiliki Triantafyllia, Joselin M Vargas, Jose D Vargas, Anurag Verma, Vibha Vij , Duane R Wesemann, Meredith Yeager, Xu Yu, Yu Zhang, Steeve Boulant, Stephen J Chanock, Jordan J Feld , Ludmila Prokunina-Olsson
Genetic regulation of OAS1 nonsense-mediated decay underlies association with COVID-19 hospitalization in patients of European and African ancestries
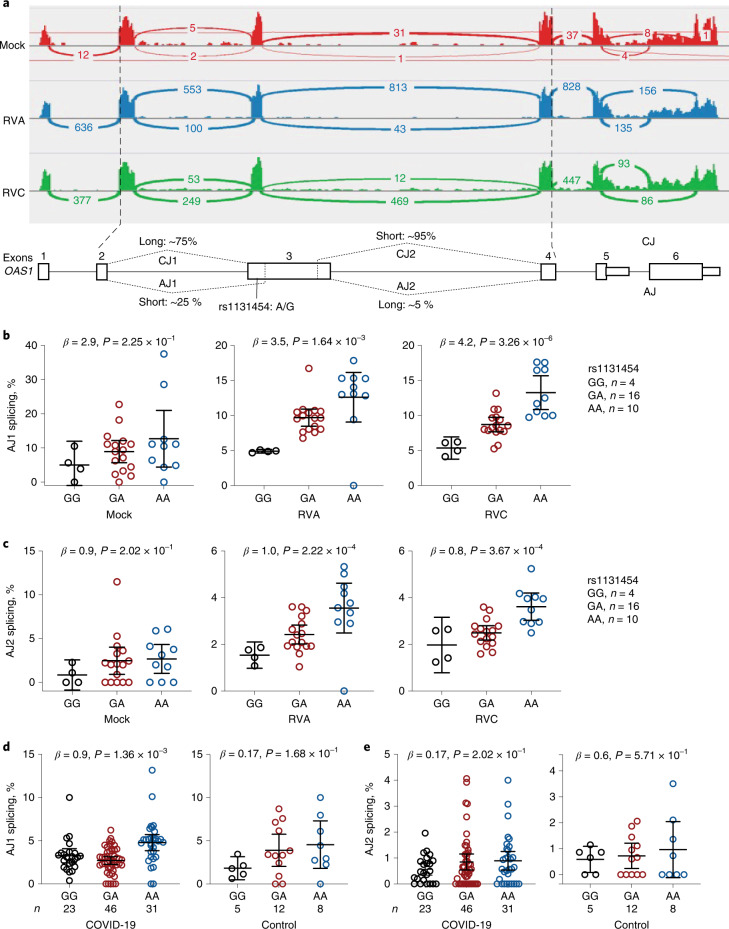
The chr12q24.13 locus encoding OAS1-OAS3 antiviral proteins has been associated with coronavirus disease 2019 (COVID-19) susceptibility. Here, we report genetic, functional and clinical insights into this locus in relation to COVID-19 severity. In our analysis of patients of European (n = 2,249) and African (n = 835) ancestries with hospitalized versus nonhospitalized COVID-19, the risk of hospitalized disease was associated with a common OAS1 haplotype, which was also associated with reduced severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) clearance in a clinical trial with pegIFN-λ1. Bioinformatic analyses and in vitro studies reveal the functional contribution of two associated OAS1 exonic variants comprising the risk haplotype. Derived human-specific alleles rs10774671-A and rs1131454 -A decrease OAS1 protein abundance through allele-specific regulation of splicing and nonsense-mediated decay (NMD). We conclude that decreased OAS1 expression due to a common haplotype contributes to COVID-19 severity. Our results provide insight into molecular mechanisms through which early treatment with interferons could accelerate SARS-CoV-2 clearance and mitigate against severe COVID-19.
Visit Journal